The 5 Big Gaps in Home Care (and how we actually fix them)
Families don’t need marketing poetry; they need care that turns up when it says it will, delivered by people who know the routine, with notes and invoices that make sense. After reviewing what people complain about most across England, we’ve boiled it down to five persistent gaps—and the concrete, measurable fixes we’ve built at Aurora Community Care.
What we looked at (methodology, plain and simple)
- Scope. On , we reviewed the Visiting Care (England) category on homecare.co.uk, then sampled 20 providers with an overall Review Score under 8.0. We read recent public reviews and, where available, cross-checked Google reviews (including aggregator surfaces like Birdeye) for the same providers.
- Why homecare.co.uk? It’s widely used in the UK and uses a 1–10 Review Score that blends average ratings with recency and volume—so a small number of fresh reviews can move a score. That “fragility” was factored into our interpretation.
- Triangulation. To separate local noise from sector-wide patterns, we also referenced independent guidance: Age UK on typical home-care complaints, and CQC guidance on medicines support & safety.
Limitations: This is a qualitative review of public feedback and guidance, not a randomized study. Still, the patterns recur with striking consistency.
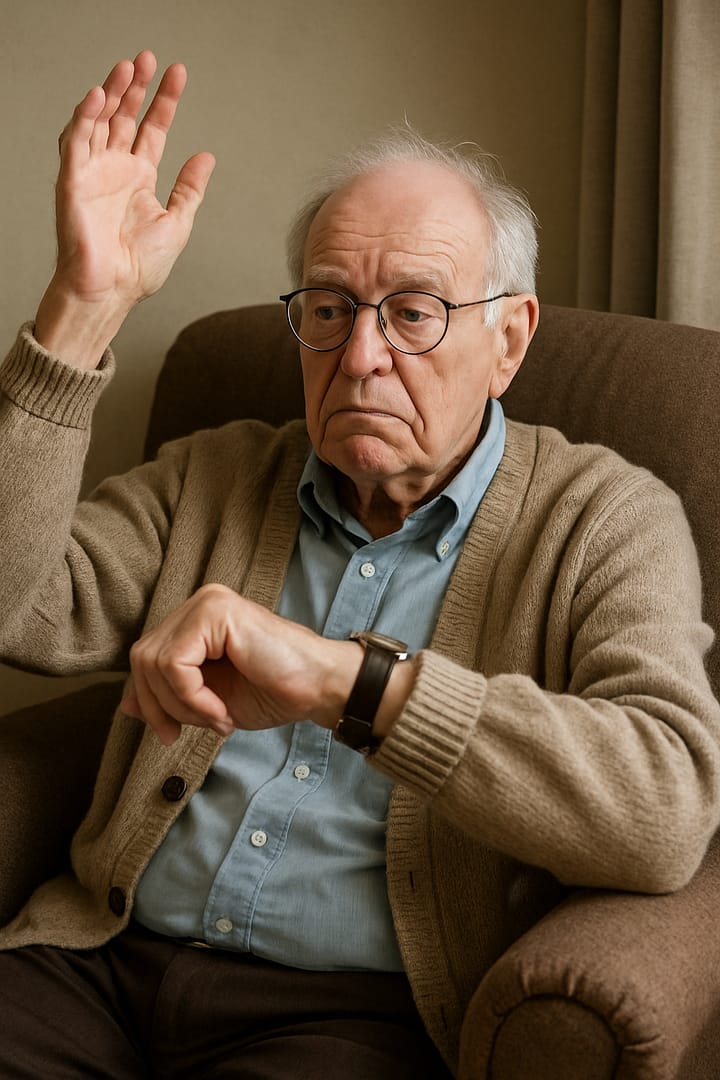
1) Unreliable visit times
What families describe: Late arrivals, missed calls, or visits squeezed so hard that essential tasks (meds, meals, personal care) get rushed.
Why it keeps happening: Over-tight rotas, long travel without buffers, and weak escalation when slippage starts.
• Time-window integrity: 95% of visits start within 20 minutes of the agreed time.
• Proactive call: we phone at +10 minutes if we’re running late—before you need to chase us.
2) Broken communication loops
What families describe: No warning on rota changes; phones ring out; notes in the app don’t match the written plan.
Why it keeps happening: Fragmented systems, no daily discipline for reconciling notes to the plan, and unclear ownership of “who phones whom when something changes.”
• Calls for changes: we phone when there’s a change to who is coming, when, or what will be done.
• Daily reconciliation: we check digital care notes against the care plan every day.
• Supervisor spot-checks: managers review updates and follow up on discrepancies the same day.
3) Low continuity of carers
What families describe: A carousel of strangers. Preferences forgotten. No relationship, no rhythm—especially tough for people living with dementia.
Why it keeps happening: Reactive scheduling, turnover, and a lack of continuity targets.
• Micro-teams (small teams): a named, stable group supports each client so faces are familiar and preferences stick.
4) Training & competency gaps
What families describe: Wobbles around medicines, dementia behaviours handled clumsily, or unsafe moving & handling.
Why it keeps happening: One-and-done induction, ad-hoc coaching, and patchy supervision.
• E-learning completion: carers complete all mandatory and relevant training (tracked electronically).
• Shadow visits: new staff shadow until both the staff member and the manager are confident they can work solo.
• Ongoing QA: regular spot-checks and supervision meetings to keep skills sharp.
5) Value & billing friction
What families describe: Care that feels “tasky and rushed” for the price—and invoices that don’t map cleanly to what actually happened.
Why it keeps happening: Generic time blocks, hidden extras, and invoices that float free of the care record.
• Invoice mirror: every line item maps to time-stamped care notes.
• Transparent pricing: everything—bank holidays, add-ons, travel—is clear before service starts.
No “goodwill credits”: we focus on delivering the service right, not papering over misses.
Why we’re confident these are the real problems
- Public reviews across England: In our 20-provider sample, the most frequent complaints cluster around punctuality, communication about rota changes, continuity of carers, and “rushed” tasks.
- Regulatory guidance: CQC stresses robust processes and competence for medicines support—exactly where timing and documentation failures show up first.
- Sector context: Oversight/inspection pressures can delay feedback loops, letting issues persist longer than anyone would like.
What you can expect from us (and how you can check)
How to verify any provider (including us)
- Ask for last month’s punctuality rate and a simple continuity measure (what % of visits were delivered by your small team).
- Ask how often care notes are reconciled to the plan—daily, weekly, or “it depends”?
- Ask to see training completion for carers on your package and when they last had observed supervision.
- Ask for a sample invoice and how each line connects to the care record.
Sources & further reading
- homecare.co.uk – Visiting Care (England) directory
- Age UK – Information & advice on home care and complaints
- CQC – Guidance for domiciliary care & medicines safety
Note: We sampled 20 sub-8.0 listings on 14 Sep 2025 and cross-checked public Google-review footprints to confirm the recurring themes.

Leave a Reply